Generalized anxiety disorder (GAD) and obsessive-compulsive disorder (OCD) are two conditions that often get confused. Both involve anxiety, but they’re not the same. GAD is defined by ongoing, excessive worry about everyday life, while OCD is marked by intrusive thoughts (obsessions) and repetitive behaviors or mental rituals (compulsions). Understanding the difference is crucial for receiving the correct diagnosis and treatment.
Read on to learn more about the signs of anxiety and OCD, how these conditions interact, and the best strategies for managing symptoms.
What is generalized anxiety disorder (GAD)?
GAD is a common anxiety disorder that about 2.7% U.S. adults experience each year. People with GAD worry excessively about everyday matters—finances, work, health, or family—even when there’s little reason to do so.
Common symptoms include:
- Excessive worry
- Restlessness
- Difficulty concentrating
- Irritability
- Sleep problems
- Heart palpitations
- Shortness of breath
- Nausea
This worry tends to be broad and shifting rather than tied to a single intrusive fear.
What is obsessive-compulsive disorder (OCD)?
OCD is a mental health condition that affects about 1 in 40 people and is defined by two main symptoms:
- Obsessions: Intrusive thoughts, images, urges, feelings, or sensations that cause significant distress (e.g., fears of harm, contamination, or acting immorally).
- Compulsions: Repetitive physical or mental acts done to relieve distress from obsessions or to prevent a feared outcome (e.g., checking, washing, reassurance-seeking).
Unlike GAD worries, OCD obsessions often are intrusive or ego-dystonic—going against the person’s values and sense of self.
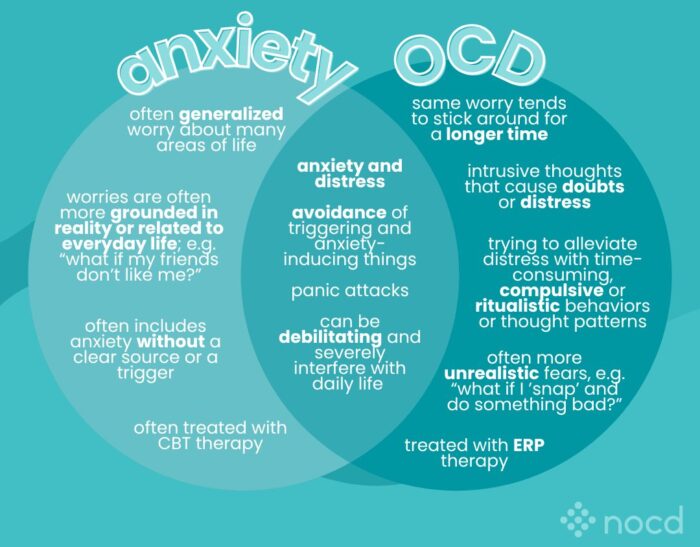
What are the key differences between GAD and OCD?
Here’s a quick comparison:
- How anxiety shows up:
- GAD → broad, shifting life worries
- OCD → specific intrusive thoughts
- Response to anxiety:
- GAD → overthinking and avoidance
- OCD → compulsions to reduce distress
- Nature of thoughts:
- GAD → worries often feel realistic, though excessive
- OCD → obsessions feel unwanted or disturbing
Can you have GAD and OCD at the same time?
Yes. Research shows that about one-third of people with OCD also meet the criteria for GAD. This overlap can complicate diagnosis—someone may experience both generalized worry and intrusive obsessions.
“Anxiety and OCD have a lot of overlap in symptoms, including physical symptoms,” says Tracie Ibrahim, LMFT, CST, Chief Compliance Officer at NOCD. She explains that people with anxiety and OCD often try to escape feelings of discomfort by avoiding the people, places, or things that trigger those feelings.
How are GAD and OCD diagnosed?
Both conditions are diagnosed through a clinical interview with a mental health professional using DSM-5 criteria.
- GAD is identified when excessive worry lasts at least six months and interferes with daily activities.
- OCD is diagnosed when obsessions and compulsions are time-consuming (more than an hour per day) or cause significant distress.
There is no blood test or scan for these disorders. Diagnosis is based on symptoms and history.
What treatments work for GAD vs. OCD?
The good news is that both GAD and OCD are manageable with the same highly effective and evidence-based treatment: exposure and response prevention (ERP) therapy. ERP is a specialized form of cognitive behavioral therapy (CBT) proven to be effective for OCD. General CBT, if not tailored for OCD, can sometimes be unhelpful or even worsen symptoms.
“It makes no difference if you have an anxiety disorder and OCD—we still do the same treatments,” explains Ibrahim. “ERP helps people learn how to face their fears, and tolerate uncertainty—allowing them to live lives where they are in control of their choices and their behaviors.”
Studies show that ERP therapy is highly effective, with 80% of people with OCD experiencing a significant reduction in their symptoms.
Other approaches that may help manage OCD and GAD include:
- Medication (typically SSRIs)
- Mindfulness-based strategies
- Acceptance and commitment therapy (ACT)
These are typically done in combination with ERP therapy, depending on the individual’s needs.
Severe or treatment-resistant OCD may benefit from the following therapies:
- Intensive outpatient programs (IOPs)
- Partial hospital programs (PHPs)
- Residential treatment centers (RTCs)
- Transcranial magnetic stimulation (TMS)
- Deep brain stimulation (DBS)
- Gamma knife radiosurgery (GKRS)
Find the right OCD therapist for you
All our therapists are licensed and trained in exposure and response prevention therapy (ERP), the gold standard treatment for OCD.
When to seek help
If anxiety or repetitive thoughts and behaviors are interfering with your relationships, work, or quality of life, it’s time to reach out for help. A mental health professional can clarify whether symptoms are best explained by GAD, OCD, or both—and guide you toward the right treatment.
Bottom line
GAD and OCD share anxiety as a common thread, but they differ in how it shows up.
- GAD → excessive, broad worry
- OCD → intrusive obsessions and compulsions
Both conditions are treatable, and the correct diagnosis makes it possible to find relief through targeted, effective care.
Key takeaways
- Anxiety disorders and OCD can look similar, but OCD is characterized by compulsions—physical or mental acts meant to relieve negative feelings.
- The presence of compulsions is what distinguishes OCD from GAD.
- GAD and OCD can occur together in the same person.
- Both anxiety and OCD are most effectively treated through ERP therapy, medications, and adjunctive therapies like ACT and mindfulness.