You are not born with fully developed obsessive-compulsive disorder (OCD), but research shows that genetics and brain differences can make some people more likely to develop the condition. Twin studies suggest that 45-65% of the risk factor for OCD is inherited, meaning family history can increase the likelihood. However, having a genetic predisposition doesn’t guarantee that someone will develop OCD—it usually requires environmental or life triggers to appear.
Continue reading to gain a deeper understanding of when OCD can develop and how effective treatment can help.
At what age does OCD usually start?
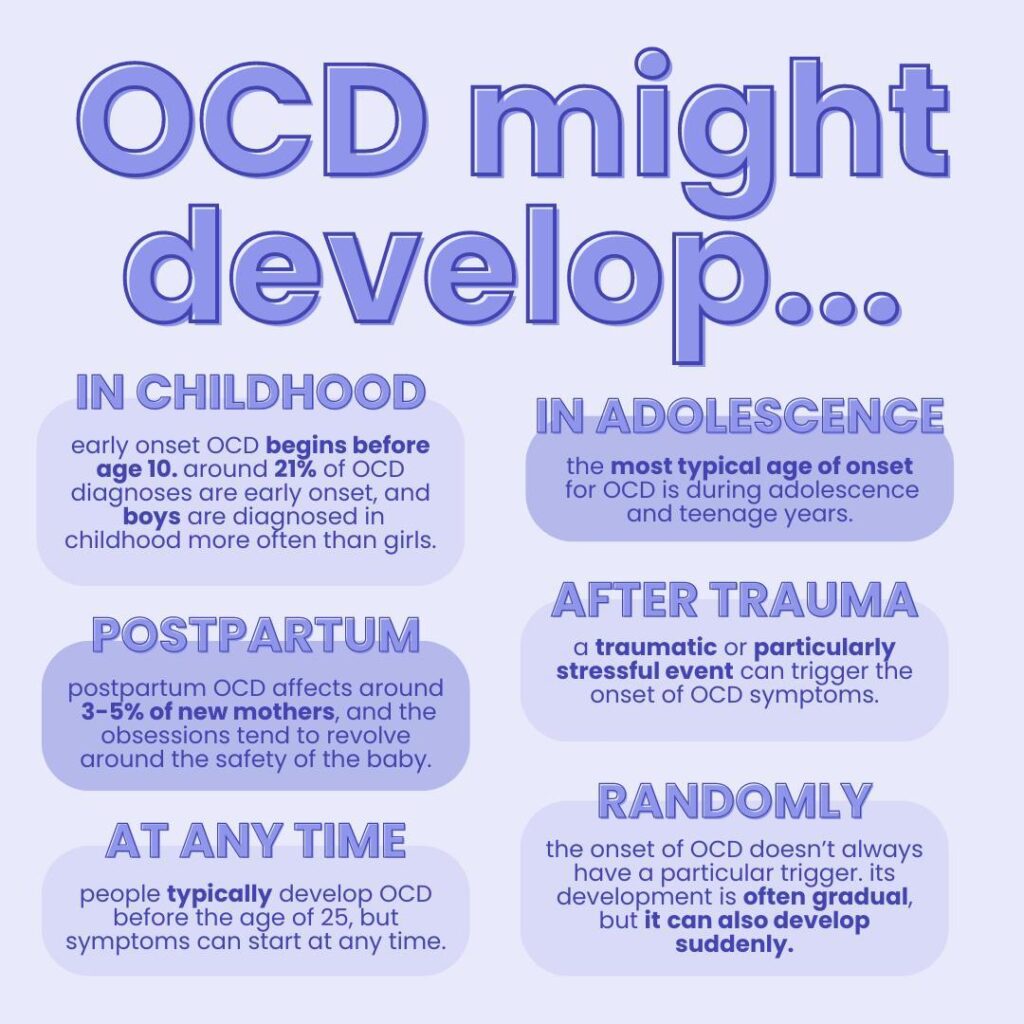
OCD typically begins in childhood, adolescence, or early adulthood. The average age of onset is around 19, but symptoms can appear as early as age 8.
There are two common onset peaks:
- Childhood-onset (8-12 years old)
- Early adult-onset (late teens to early 20s)
Once symptoms appear, they tend to persist without treatment. Early recognition and therapy can help prevent OCD from becoming more severe over time.
Can you develop OCD later in life?
Yes, OCD can develop in adulthood, even in people with no prior symptoms. While less common, late-onset OCD may appear in the 30s, 40s, or beyond. Triggers can include stressful life events, hormonal changes, or co-occurring mental health conditions. In rare cases, neurological changes like head trauma or neurodegenerative conditions may also play a role.
Adults who develop OCD later in life often experience the same obsessions and compulsions as younger individuals, though their symptoms may center on health, morality, or family-related fears.
What causes OCD to develop?
OCD is thought to arise from a combination of:
- Genetics: Family history increases risk.
- Brain differences: Research shows changes in brain circuits related to decision-making and fear regulation.
- Environment: Stressful or traumatic events can trigger symptoms.
- Medical factors: Conditions such as PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections) may trigger OCD in children.
No single factor “causes” OCD—instead, it results from an interaction of biological factors and life experiences.
Does OCD go away on its own?
OCD rarely goes away without treatment. Symptoms often worsen during periods of stress, and delaying treatment can make recovery more challenging.
The most effective treatment for OCD is exposure and response prevention (ERP) therapy. ERP is a specialized form of cognitive behavioral therapy (CBT) proven to be effective for OCD. General CBT, if not tailored for OCD, can sometimes be unhelpful or even worsen symptoms.
Studies show that ERP therapy is highly effective, with 80% of people with OCD experiencing a significant reduction in their symptoms.
Other approaches that may help include:
- Medication (typically SSRIs)
- Mindfulness-based strategies
- Acceptance and commitment therapy (ACT)
These are typically done in combination with ERP therapy, depending on the individual’s needs.
Severe or treatment-resistant OCD may benefit from the following therapies:
- Intensive outpatient programs (IOPs)
- Partial hospital programs (PHPs)
- Residential treatment centers (RTCs)
- Transcranial magnetic stimulation (TMS)
- Deep brain stimulation (DBS)
- Gamma knife radiosurgery (GKRS)
Find the right OCD therapist for you
All our therapists are licensed and trained in exposure and response prevention therapy (ERP), the gold standard treatment for OCD.
Bottom line
You are not born with OCD in the way you’re born with eye color, but genetics and brain biology can predispose you to it. Symptoms usually begin in childhood or early adulthood, but OCD can also occur later in life due to environmental stressors or medical factors. Regardless of when it starts, OCD is a treatable condition, and effective therapies are available at any age.
Key takeaways
- You are not born with OCD, but genetics and brain biology can increase your risk.
- OCD most often begins in childhood, adolescence, or early adulthood, with an average onset around age 19.
- While less common, OCD can also develop later in life, sometimes triggered by stress, trauma, or medical changes.
- OCD rarely goes away on its own, but evidence-based treatments like ERP therapy and medication can lead to major improvement.